Major Depressive Disorder (MDD) is a common but serious mental health condition. It affects millions of people worldwide. MDD causes long-lasting sadness, low motivation, and loss of interest in activities. These symptoms can make daily life difficult.
The good news is that effective medications can help manage MDD. They support people on their path to recovery. If you or a loved one is thinking about using medication, learning about the options, how they work, and possible side effects can help you make informed choices.
Before starting this topic, check out our previous blog post, How to Treat Obsessive-Compulsive Disorder (OCD). It will help explore the various approaches for treating OCD.
Types of Medications for Major Depressive Disorder (MDD)
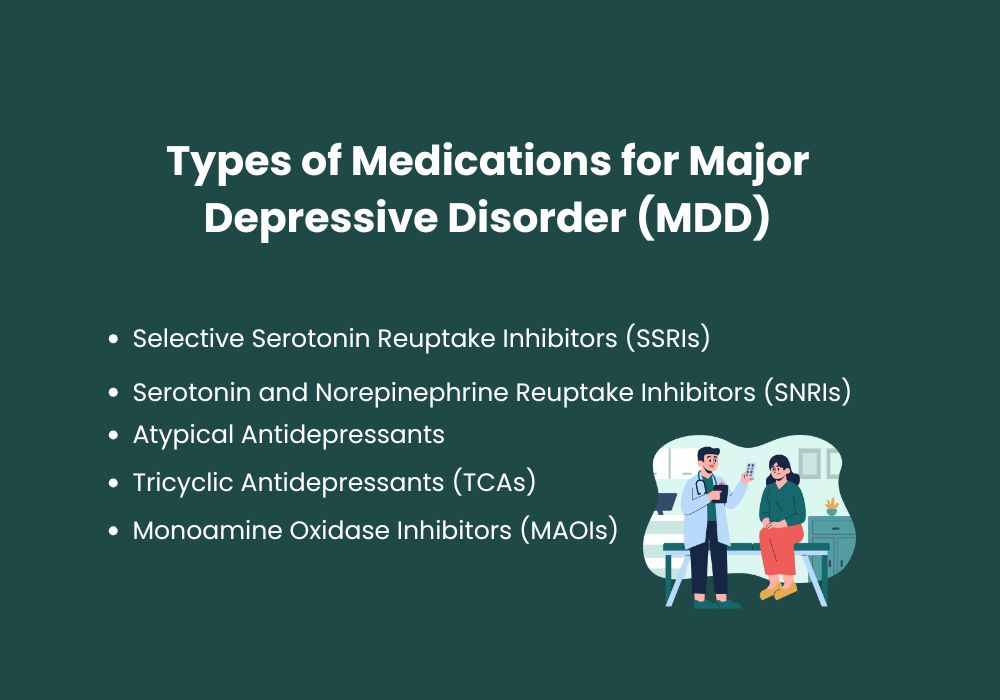
Several types of medications are used to treat Major Depressive Disorder (MDD). Each type affects brain chemicals, called neurotransmitters, that help control mood. They can work in different ways for different people. Common categories of these medications include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are often the first choice for treating depression. They help by boosting serotonin levels in the brain, which can lift mood and ease anxiety. Popular SSRIs include:
- Fluoxetine (Prozac)
- Sertraline (Zoloft)
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Paroxetine (Paxil)
What to Expect: SSRIs usually take about 4 to 6 weeks to reach their full effect. Many people notice they feel more balanced and less anxious during this time.
Common side effects can include nausea, headaches, and sleep problems. These side effects often get better as the body adjusts to the medication.
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs are another class of antidepressants that affect both serotonin and norepinephrine levels. They’re handy for people who haven’t responded to SSRIs. Common SNRIs include:
- Venlafaxine (Effexor)
- Duloxetine (Cymbalta)
What to Expect: SNRIs can help boost energy, improve mood, and enhance focus and concentration. Some side effects may occur, such as higher blood pressure, dry mouth, and dizziness. Like SSRIs, SNRIs usually take several weeks to show their full benefits.
Atypical Antidepressants
This category includes medications that don’t fit neatly into other categories but can be highly effective for some individuals. Examples include:
- Bupropion (Wellbutrin): Often chosen when other antidepressants cause sexual side effects or fatigue, as it generally doesn’t have these issues.
- Mirtazapine (Remeron): Sometimes prescribed for individuals with insomnia or significant weight loss.
What to Expect: Atypical antidepressants work in different ways depending on the specific medicine. Bupropion can help boost energy and improve focus. Mirtazapine may help with sleep and regulate appetite.
Possible side effects include trouble sleeping for bupropion and weight gain for mirtazapine. Knowing these effects can help you manage them and work with your doctor to find the right medication.
Tricyclic Antidepressants (TCAs)
One of the older classes of antidepressants, TCAs are less commonly prescribed today due to potential side effects, but can be effective for treatment-resistant depression. Common TCAs include:
- Amitriptyline
- Nortriptyline (Pamelor)
- Imipramine (Tofranil)
What to Expect: TCAs may improve mood, sleep, and pain symptoms. Possible side effects include dry mouth, constipation, and dizziness. Due to potential side effects, these medications usually require close monitoring.
Monoamine Oxidase Inhibitors (MAOIs)
MAOIs are not used very often today because they require strict dietary restrictions. Eating certain foods or taking some other medications while on MAOIs can cause serious health problems. Despite this, MAOIs can still help people with atypical or treatment-resistant depression. Examples of these medications include:
- Phenelzine (Nardil)
- Tranylcypromine (Parnate)
What to Expect: MAOIs can be highly effective, but users must avoid foods high in tyramine (like certain cheeses and cured meats) to prevent dangerous increases in blood pressure. Common side effects are feeling dizzy and gaining weight.
Starting Medication for Major Depressive Disorder (MDD): What You Should Know
- The Timeline of Effects: Antidepressants usually take several weeks to start working. Many people notice some improvement within 2 to 4 weeks. Full benefits may take up to 12 weeks. Early changes can include better sleep and a healthier appetite, while improvements in mood and motivation often take longer.
- Managing Side Effects: Mild side effects are common when starting an antidepressant. These can include nausea, headaches, or drowsiness. Most side effects improve after a few weeks. If side effects continue or are bothersome, your psychiatrist may adjust the dose or suggest a different medication.
- Staying Consistent: Adhering to a regular medication schedule is crucial for effective treatment. Stopping antidepressants suddenly can cause withdrawal symptoms such as dizziness or irritability. It may also bring back depression symptoms. Always consult your healthcare provider before changing or stopping medication.
- The Importance of Monitoring and Follow-up: Regular visits with your psychiatrist are very important, especially during the first few months. These appointments allow your doctor to monitor your progress, adjust medication doses as needed, and address any concerns or side effects. Open communication helps make sure your treatment plan meets your needs.
Medication as Part of a Comprehensive Treatment Plan

While medications can significantly alleviate MDD symptoms, they are often most effective when combined with other treatments. A holistic approach to managing MDD typically includes:
- Psychotherapy: Cognitive Behavioral Therapy (CBT) is one of the most effective forms of talk therapy for MDD. CBT helps patients identify and challenge negative thought patterns and develop healthier ways of coping with stress and emotions.
- Lifestyle Adjustments: Regular exercise, a balanced diet, and adequate sleep can all play a role in supporting mental health.
- Support Networks: Joining a support group or connecting with friends and family members who understand MDD can provide emotional support and reduce feelings of isolation.
Myths and Facts about Antidepressant Medications for Major Depressive Disorder (MDD)
Myth: Antidepressants change your personality.
Fact: Antidepressants work to balance chemicals in the brain to reduce depressive symptoms. They do not alter personality traits, but they may make people feel more like themselves by reducing depression symptoms.
Myth: Antidepressants are addictive.
Fact: Unlike addictive substances, antidepressants do not create a craving or compulsive behavior. However, stopping them suddenly can lead to withdrawal symptoms, which is why gradual tapering is advised.
Myth: Once you start medication, you’ll be on it for life.
Fact: The length of time someone needs to take antidepressants varies. Some people use them for a few months, while others may need longer-term treatment. Your psychiatrist will work with you to find the best plan.
When to Talk to Your Psychiatrist for Major Depressive Disorder (MDD)
If you notice new or worsening symptoms, unusual side effects, or changes in your mood, it is important to talk with your psychiatrist.
If your medication does not provide enough relief after a proper trial period, your doctor may suggest other options. There are many types of antidepressants available, and finding the right one can take time.
Being patient and working closely with your healthcare provider is worth it for long-term mental wellness and overall quality of life.
Conclusion
For people dealing with Major Depressive Disorder, medications can provide an important lifeline. They help manage symptoms and support recovery.
Knowing what to expect, handling side effects, and following your treatment plan consistently all help make the process more effective. With guidance from a caring psychiatrist and the right support, finding relief from MDD is possible.
At Peniel Psychiatry, we are here to help you on your journey to better mental health. Reach out today to discover how we can support your path to wellness.




